Your cart is currently empty!
Category: Health Insurance
Does Insurance Cover Chiropractic During Pregnancy?
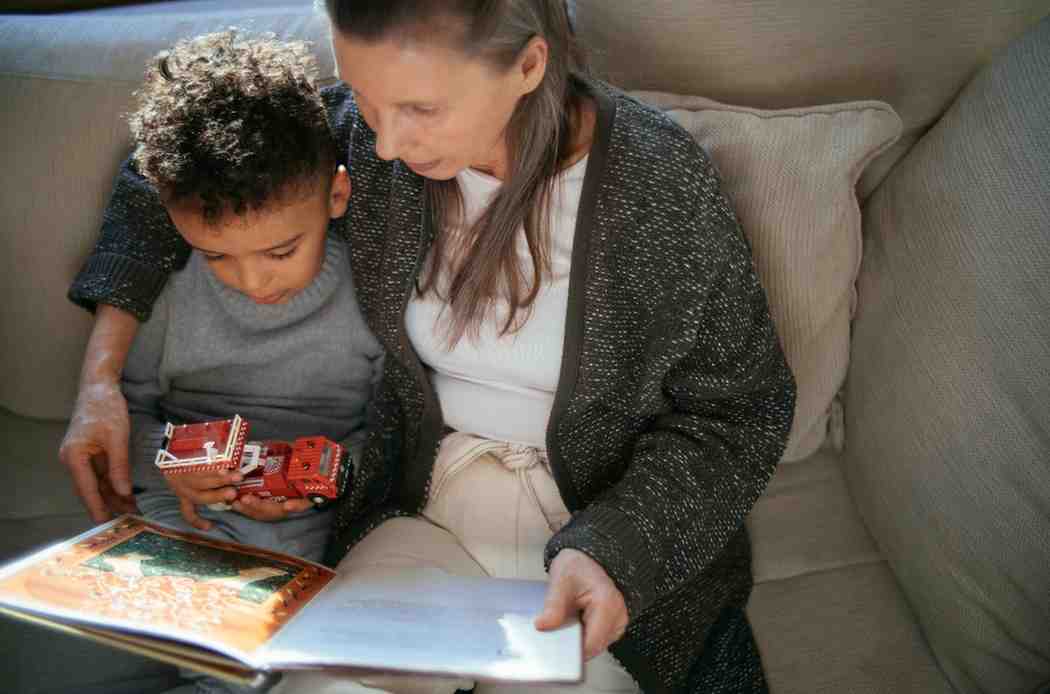
Pregnancy is a unique journey filled with excitement, anticipation, and, for many, unexpected discomfort. As the body changes to support a growing baby, expectant mothers often turn to chiropractic care for relief from back pain, pelvic discomfort, and sciatic nerve issues.
But one question is common among moms-to-be: Does insurance cover chiropractic care during pregnancy? The answer depends on your plan, your provider, and how the services are billed.
Why Pregnant Women Seek Chiropractic Care
During pregnancy, your body undergoes hormonal shifts and physical changes that can cause discomfort. Chiropractic care is a hands-on approach that focuses on spinal and pelvic alignment to improve comfort, reduce pain, and support better overall function.
Common Reasons for Chiropractic Visits During Pregnancy
- Back Pain Relief: As the belly grows, it puts strain on the lumbar spine, leading to chronic aches.
- Pelvic Balance: Proper alignment can reduce pressure and may help with positioning the baby for birth.
- Sciatica: Some pregnant women experience shooting pain down the legs caused by sciatic nerve pressure.
When I was pregnant with my second child, I experienced intense lower back pain that made it hard to get out of bed. A friend suggested her prenatal chiropractor. I was skeptical at first, but within a few sessions, I noticed less pain and better mobility—especially in my hips and lower back.
If you’re exploring various wellness services, you might also be curious about massage therapy coverage or does insurance cover acupuncture—both popular options for holistic pregnancy care.
Is Chiropractic Care Covered by Insurance?
Most insurance plans offer limited coverage for chiropractic care under general wellness or rehabilitative services. However, that doesn’t always mean they cover it during pregnancy.
Coverage Often Depends on Several Factors
- The Insurance Policy: Some policies include a fixed number of visits per year.
- Medical Necessity: You may need a doctor’s referral, especially from your OB-GYN.
- In-Network Providers: Visiting a provider in your insurer’s network helps keep out-of-pocket costs low.
- State Programs Like Medicaid: Depending on your state, Medicaid may cover prenatal chiropractic care if it’s considered medically necessary.
If you’re enrolled in an ACA plan, you can review maternity benefits and learn what’s included by visiting the Marketplace website.
For other maternity-related insurance topics, check out:
How to Find Out If Your Insurance Covers It
Call Your Insurance Provider
The number on the back of your insurance card is your best bet. Ask specific questions like:
- Is chiropractic care covered for pregnancy-related pain?
- Is a referral required?
- How many visits are allowed per year?
- What are the out-of-pocket costs?
Review Your Plan’s Explanation of Benefits
Your insurance provider’s website usually has a PDF of your Explanation of Benefits (EOB), which outlines what’s covered and what’s not. Understanding terms like coinsurance, deductibles, and copays is essential.
Want to know how this process works for other services? See how to verify chiropractic coverage.

What If Insurance Doesn’t Cover It?
If your policy doesn’t offer prenatal chiropractic coverage, you still have options.
Out-of-Pocket Payment Plans
Many chiropractors offer discounted packages if you’re paying without insurance. Be upfront and ask about flexible pricing.
Use an HSA or FSA
Funds from a Health Savings Account (HSA) or Flexible Spending Account (FSA) can often be used to pay for chiropractic visits.
Seek Community Health Resources
Local programs or nonprofit clinics may provide affordable chiropractic services for expectant mothers. You can also research programs that help cover low-income pregnancy services.
Benefits of Chiropractic Care During Pregnancy
For many expectant moms, chiropractic adjustments offer more than pain relief.
Common Benefits Include:
- Less back and hip pain
- Better sleep quality
- More comfortable walking and standing
- Potential for smoother labor and delivery
My chiropractor explained how pelvic alignment helps the baby settle into the right position. Knowing that something so simple could potentially ease my labor made the appointments feel even more worthwhile.
If you’re exploring broader coverage options, learn about prenatal insurance for high-risk pregnancies and how to find insurance plans with maternity benefits.
Understanding the Webster Technique
The Webster Technique is a specialized chiropractic method designed for pregnancy. It focuses on aligning the pelvis and reducing tension in surrounding muscles and ligaments.
This technique is especially popular for cases where the baby is breech. While it doesn’t guarantee a head-down position, some studies suggest it may increase the likelihood of turning the baby.
Ask your chiropractor if they are certified in this method before booking an appointment.
Tips for Choosing the Right Chiropractor
- Make sure they are trained in prenatal care
- Look for certification in the Webster Technique
- Read reviews or ask for recommendations
- Ensure they are covered by your insurance network
You might also be interested in understanding what your policy says about alternative therapies during pregnancy or what to do if insurance denies maternity claims.
Final Thoughts
Chiropractic care during pregnancy can be a major help for managing the physical demands of carrying a baby. While not all insurance plans cover it, taking the time to check your policy, ask questions, and explore your options can help you make an informed decision.
From my own experience, I can confidently say that it made my pregnancy much more manageable—and even enjoyable. Whether your visits are covered by insurance or paid out-of-pocket, the support chiropractic care provides during pregnancy is often worth the investment.
FAQs
Is chiropractic care safe during pregnancy?
Yes, when performed by a trained prenatal chiropractor, it’s considered safe and effective.How much does it cost without insurance?
Prices vary but generally range from $50–$200 per session, depending on your location and the chiropractor’s experience.Can chiropractic care make labor easier?
Some moms report shorter and smoother labors after regular chiropractic care, especially when focused on pelvic alignment.
Spot Pet Insurance Pros and Cons Explained
Owning a pet is one of the most rewarding experiences, but it can come with unexpected costs. When my dog, Bella, got sick last year, the vet bills piled up quickly. This is when I realized how important pet insurance could be. Spot Pet Insurance is one of the companies offering coverage that helps protect pet owners from unexpected medical expenses.

What Is Spot Pet Insurance?
Spot Pet Insurance helps cover the cost of your pet’s medical care. Whether it’s an accident or illness, Spot offers plans that cover a variety of treatments and services. This can be a lifesaver for pet owners who want to avoid high vet bills.
Key Features of Spot Pet Insurance
Types of Coverage Offered
Spot offers two main types of plans:- Accident-Only Coverage: This covers treatment if your pet is injured in an accident (like broken bones or bites).
- Accident and Illness Coverage: This more comprehensive plan covers illnesses like infections, digestive issues, or chronic conditions.
Optional Add-Ons
Spot also has a wellness plan you can add. This helps with routine care costs like vaccinations and check-ups. When Bella needed her annual shots, having this kind of add-on would have helped a lot.Customizable Plans
You can choose the deductible (the amount you pay before insurance kicks in) and the annual limit (the most your insurance will pay out in a year). This makes it easier to create a plan that fits your budget.Why Choose Spot Pet Insurance?
Flexible Options
Spot gives pet owners the chance to customize their plans. When I was researching insurance for Bella, I liked how I could pick a plan that covered just the basics or go for one that included more.Choose Any Vet
With Spot, you don’t have to stick to a specific network. You can go to any licensed vet, which was great for me since Bella’s favorite vet isn’t part of a big chain.Easy Claims Process
Filing a claim with Spot is pretty straightforward. You submit your bill online and wait for reimbursement. This can be very helpful when facing sudden expenses, like when my friend’s cat, Luna, needed an emergency visit for a cut on her paw.Also Read: Top Pet insurance companies
How Much Does Spot Pet Insurance Cost?
Factors Affecting Cost
The price you pay for Spot insurance depends on things like your pet’s age, breed, and where you live. Bigger dogs or certain breeds might cost more to insure. When I looked into it, I saw that younger pets tend to have lower premiums.Example Costs
For a small, young dog, a basic plan might cost around $25 a month. For a larger, older dog, it could go up to $50 or more per month. The more coverage you add, the higher the cost, but it’s worth it for peace of mind.Discounts
Spot sometimes offers discounts for insuring more than one pet. If I ever adopt a second dog, this could be a great way to save money.
Pros and Cons of Spot Pet Insurance
Pros Cons Customizable plans to fit different needs Does not cover pre-existing conditions Easy-to-use and accessible claims system Has waiting periods before coverage begins No age limits for enrollment Costs can be higher for older pets or certain breeds Freedom to choose any licensed vet Some exclusions may apply (e.g., certain treatments) Comparing Spot Pet Insurance to Other Providers
When I was comparing insurance for Bella, I also looked at Healthy Paws and Embrace. Spot stood out for its flexibility and customer service. While Healthy Paws has a good reputation, it didn’t have the same customization options I liked about Spot.
You may interested: Pet Care Business
How to Enroll in Spot Pet Insurance
Easy Sign-Up Process
Signing up is simple. You fill out basic information about your pet online, choose your plan, and pay the first premium. I found it quick when I tried signing up out of curiosity for Bella.Documents You Need
Usually, you just need details like your pet’s age and medical history. It helps to have recent vet records handy.Choosing the Right Plan
Think about your budget and how much coverage you want. I always recommend looking at a few options and comparing them side by side.What Do Customers Say About Spot?
Most people like Spot’s easy claims process and flexible coverage options. Some mention that they got their reimbursements quickly, which is a huge plus.
However, some complaints are about specific exclusions or waiting periods. Personally, if I decide to get coverage for Bella, I’d keep these in mind.
In Short
Spot Pet Insurance is a solid choice for pet owners who want peace of mind. Whether it’s for a young pup or an older cat, having coverage means less worry when those unexpected vet bills pop up. For me, knowing Bella could be protected in case of an emergency is a big relief.
If you’re thinking about getting insurance, check out Spot’s options and see if they fit what you need.
FAQs
1. What about pre-existing conditions?
Spot doesn’t cover pre-existing conditions. This is why it’s good to enroll when your pet is still healthy.2. How long does it take to get reimbursed?
Typically, it takes around 7-10 days after your claim is approved.3. Can I cancel my policy?
Yes, you can cancel anytime, but make sure to read the fine print about refunds.
How Is Physical Therapy Reimbursed by Insurance?
Navigating the process of getting physical therapy reimbursed by insurance can feel overwhelming. With so many different types of coverage, eligibility requirements, and rules to follow, it’s easy to see why some people avoid physical therapy altogether due to potential costs.

Here’s a breakdown of how insurance reimbursement for physical therapy typically works and what to expect at each step—along with a few personal tips to make it feel less daunting.
Physical Therapy Costs and Insurance Reimbursement
Physical therapy can be a real lifeline for people recovering from surgeries, injuries, or chronic pain. But the cost of regular sessions adds up quickly. Insurance plays a major role in making this crucial healthcare service accessible. The goal of insurance reimbursement is to help people afford physical therapy that can improve their quality of life, restore mobility, and reduce pain. Without insurance coverage, the price can sometimes be prohibitive, especially for long-term treatments.
I remember when a family member needed physical therapy after a knee surgery. Initially, we were unsure if insurance would cover enough of it to make it affordable. But knowing what questions to ask and understanding the insurance process made a huge difference.
Also Read: Massage Therapy Coverage
Types of Insurance Coverage for Physical Therapy
There are several types of insurance that may cover physical therapy, each with its own set of rules and limitations. Here’s a quick look:
- Private Health Insurance: Most private health insurance plans, like PPOs and HMOs, offer some level of coverage for physical therapy. However, the specifics—such as the number of sessions covered, in-network provider requirements, and co-pays—vary significantly between providers. Some plans require a pre-authorization before they cover any costs.
- Government-Sponsored Insurance: Medicare and Medicaid also cover physical therapy but with different stipulations:
- Medicare: Typically covers medically necessary physical therapy if prescribed by a physician. However, there are caps on the amount reimbursed annually.
- Medicaid: Coverage for physical therapy under Medicaid depends on state regulations. Some states offer generous benefits, while others may have stricter limits or may require co-pays.
- Workers’ Compensation: If the need for physical therapy is related to a workplace injury, workers’ compensation often steps in to cover costs. The process for approval here can be simpler since it’s directly linked to the injury sustained on the job.
- Auto Insurance: If physical therapy is required following a car accident, some auto insurance policies include provisions for medical treatment like physical therapy.
Eligibility Criteria for Reimbursement
One of the most important things to understand about insurance reimbursement for physical therapy is eligibility. Insurance companies require certain conditions to be met before they cover therapy sessions.
- Medical Necessity: Insurance companies are strict about “medical necessity.” This means the therapy has to be essential for treating a specific condition diagnosed by a medical professional. A doctor’s recommendation alone isn’t always enough; sometimes, additional documentation or evidence may be needed.
- Pre-Authorization Requirements: Some plans require pre-authorization to confirm that the treatment is eligible for coverage. Failing to obtain pre-authorization can lead to claim denials, so always check this with your insurer. In my family member’s case, I made sure we got pre-authorization for each stage of therapy, which saved us a lot of hassle later.
- Referral from Healthcare Providers: Many insurers require a referral from a primary care physician. This step can help ensure the insurance covers as many sessions as needed. If the insurer deems the therapy excessive or unnecessary, it might deny the reimbursement request, so a clear medical recommendation is key.
Key Insurance Terms to Know
Term What It Means Medical Necessity PT must be essential for your condition to get coverage Pre-Authorization Approval some insurers need before paying for PT In-Network Provider Therapist your insurer covers at a better rate Deductible Amount you pay before insurance kicks in Co-pay Set fee you pay at each visit Explanation of Benefits A summary of what insurance paid and what you owe The Reimbursement Process for Physical Therapy
Once eligibility is confirmed, the next step is to understand how the reimbursement process works.
- Filing Claims: Filing an insurance claim can often be done by the clinic where you’re receiving physical therapy, but it’s still helpful to know how it works. The clinic typically submits treatment documentation and billing codes to the insurer, who then processes the claim and determines how much will be reimbursed.

- Explanation of Benefits (EOB): After filing a claim, insurers send an EOB statement. This details how much they paid for each session and what portion is the patient’s responsibility. At first, EOBs might look confusing, but they’re crucial for understanding insurance coverage. I learned to read EOBs line-by-line to catch any errors or unexpected charges.
- Billing and Coding: Physical therapy services are billed using specific codes, and accurate coding is essential for successful reimbursement. Incorrect or outdated codes are one of the top reasons for claim denials, so working with a knowledgeable clinic is essential.
Factors Affecting Reimbursement Amounts
Even with approval, several factors influence how much of the physical therapy cost will actually be covered:
- Insurance Plan Limits: Insurance plans often have a maximum reimbursement amount or limit the number of sessions. For instance, some policies cap coverage at 20 visits per year. Knowing these limits can help in planning treatment effectively.
- Co-pays, Deductibles, and Co-insurance: Out-of-pocket costs are an unavoidable part of insurance. These costs vary by plan and can sometimes make physical therapy feel unaffordable. My tip: ask the clinic for an estimate of what your insurance will cover before treatment begins.
- In-Network vs. Out-of-Network Providers: Insurance companies typically offer better reimbursement rates if you use an in-network provider. Out-of-network providers may still be covered, but at a lower rate, leaving you with more to pay out-of-pocket.
Common Challenges and Solutions in Physical Therapy Reimbursement
Dealing with insurance companies can bring challenges. Here are a few common ones:
- Denials and Appeals: Sometimes, claims are denied. This can happen if a treatment is deemed unnecessary, improperly coded, or lacks the right documentation. The good news is that many denials can be appealed. I’ve found that gathering all relevant documentation and working closely with the clinic increases the chances of a successful appeal.
- Underpayment or Partial Reimbursement: Sometimes insurers only partially cover sessions, and getting them to pay the full amount can be frustrating. One way to address this is to contact the insurance company and review the EOB to see where the discrepancy might be.
- Changing Coverage Regulations: Insurance companies frequently update their policies. It helps to stay informed, especially if you or a family member needs ongoing therapy.
Tips for Maximizing Physical Therapy Reimbursement
- Choose an In-Network Provider: It may sound simple, but choosing an in-network provider can drastically reduce costs. I learned this the hard way when our initial physical therapist was out-of-network, which doubled our expenses.
- Review Your Insurance Policy: Reviewing the policy is essential for maximizing coverage. Knowing exactly what your plan covers and when to request pre-authorizations or referrals can prevent unwelcome surprises.
- Communicate with Your Insurance Company: Keeping an open line with your insurer ensures smoother reimbursement. If something’s unclear, don’t hesitate to call. Ask questions about specific policies and steps to avoid any missteps along the way.
In Short
Getting physical therapy reimbursed by insurance can be a complicated journey, but being prepared helps. By understanding the types of insurance, eligibility requirements, and reimbursement process, you can better navigate the complexities of insurance and get the care you need. With a little bit of planning, and by taking proactive steps, insurance can make physical therapy more accessible, so you or your loved ones can focus on healing and getting back to a full, healthy life.

AICPA Life Insurance Guide with Benefits and How to Cancel
When it comes to financial planning, life insurance often stands as one of the most important, yet challenging, pieces of the puzzle. AICPA Life Insurance, offered by the American Institute of CPAs (AICPA) and underwritten by Prudential, specifically caters to CPAs and their families, providing a unique set of benefits and flexible plans.

Let’s dive into what makes AICPA Life Insurance distinct, who it’s best suited for, and how to cancel it if your life circumstances change.
Feature Details Provider AICPA, underwritten by Prudential Types of Policies Group Term, Spouse, Family, Child Coverage Pros Affordable, flexible options, trusted Cons Limited customization, term only, exclusive How to Cancel Contact support, submit forms, confirm What Is AICPA Life Insurance?
AICPA Life Insurance is a specialized group life insurance program available exclusively for AICPA members and their families. Offered through a partnership with Prudential, it allows CPAs access to competitively priced life insurance options tailored to their specific needs.
I remember first learning about AICPA Life Insurance when I was starting my career. Life insurance wasn’t top of mind, but I’d heard how important it was for financial security. With AICPA, the peace of mind was immediate; it felt secure to know I had a backup plan at an affordable rate, which was a relief, especially when funds were tight in those early years.
Types of AICPA Life Insurance Policies
AICPA offers different types of life insurance options, ensuring members have the flexibility to choose what fits them best. Here are the main types available:
- Group Term Life Insurance: This is the standard plan, ideal for those seeking solid, basic life insurance protection.
- Spouse and Family Life Insurance: A convenient option to protect spouses and other family members under the same plan.
- Child Life Insurance: Provides coverage for children, giving parents a level of reassurance against unexpected events.
Benefits of AICPA Life Insurance
AICPA Life Insurance offers several advantages over typical market policies, such as:
- Lower Premium Rates: AICPA leverages group rates, which can significantly lower premiums, especially compared to private plans.
- Flexibility in Coverage: From basic term life to family plans, there’s something for everyone.
- Stability and Trust: Being backed by AICPA and Prudential adds an extra layer of trustworthiness and stability.
Eligibility and Requirements
Eligibility for AICPA Life Insurance is straightforward but exclusive to CPAs and their families. Proof of AICPA membership and identification documentation are generally required during enrollment. Family members, such as spouses and children, can also be added as dependents. It’s particularly helpful for CPAs who may not have insurance coverage from their employers, allowing them to secure affordable coverage independently.
AICPA Life Insurance Coverage Options and Features
Understanding the different coverage options is essential when considering AICPA Life Insurance. Each option serves a unique purpose, and it’s worth weighing them carefully.
Group Term Life Insurance
This plan is designed to be the primary life insurance option for AICPA members. It offers coverage that can be renewed annually, making it an affordable choice for short-term needs or younger members who may upgrade their policies later.
Additional Life Insurance Options
Spouse, family, and child insurance plans provide additional flexibility. These are popular among CPAs with families since it’s convenient to keep everyone on one policy. I’ve personally found this helpful—having a consolidated plan for my spouse and children keeps everything organized and ensures I’m not juggling multiple policies.
Also Read: Young America Insurance
Key Policy Features
One of the biggest perks is that AICPA Life Insurance policies come with flexible premiums and renewal options, allowing members to adjust coverage as their needs change. Whether you’re early in your career or preparing for retirement, AICPA Life Insurance can adapt to different stages of life, though it’s best suited for term coverage, not permanent insurance.
How to Cancel AICPA Life Insurance
Life circumstances change, and sometimes that means your insurance needs do too. Here’s a breakdown of the process for canceling AICPA Life Insurance.
Reasons to Consider Cancelling
Some of the main reasons people cancel AICPA Life Insurance include lifestyle changes, better coverage options, or financial adjustments. In my own experience, I reevaluated my insurance needs when I started building more savings and wanted a permanent policy that could grow with my assets. AICPA Life Insurance is great for early financial planning, but it may not meet all long-term goals.
Cancellation Process
To cancel AICPA Life Insurance, here’s what to do:
- Contact AICPA or Prudential Support: Call their customer service line or log in to your online account to request cancellation.
- Submit Required Documents: Often, some paperwork or verification is needed to complete the process.
- Confirm Cancellation: Double-check that your policy has been successfully canceled to avoid unexpected charges.
The process is straightforward, but it’s wise to plan ahead so you don’t accidentally go uninsured. After I canceled my own AICPA policy, I went through an assessment period to figure out the best replacement, this allowed me to make a smooth transition without lapses in coverage.

Alternatives and Next Steps After Cancellation
If you’re canceling, it’s essential to look into replacement policies right away. Individual life insurance policies can be beneficial as they often offer customizable terms and benefits. Consider consulting a financial advisor to explore options for personal life insurance or permanent coverage if you’re planning to cancel.
Pros and Cons of AICPA Life Insurance
Every life insurance plan has its upsides and downsides. Here are a few to keep in mind with AICPA’s offerings.
Pros Cons Affordable Premiums – Group pricing offers lower costs compared to individual plans. Limited Customization – Group plan options lack personalization. Trustworthy Partnership – Backed by AICPA and underwritten by Prudential for reliability. No Permanent Coverage – Focuses on term life, not ideal for long-term needs. Flexible Coverage Options – Options for term life, family, and child insurance plans. Exclusivity – Only available to AICPA members and their families. Final Thoughts
AICPA Life Insurance is a valuable option for CPA professionals, especially for those looking for affordable, reliable coverage early in their careers. With its focus on term coverage, it may not suit everyone’s long-term needs, but for those seeking flexibility and group rates, it’s worth exploring.
If you’re considering cancellation, weigh your options carefully and make sure you have a new policy ready to go if needed. It’s often during these transitional periods that careful planning can ensure your financial future stays secure. Whatever stage of life you’re in, understanding your insurance options can help you make the best choice for your unique circumstances.
Open Care Life Insurance affordable coverage insights
When it comes to life insurance, making the right choice can feel overwhelming. With so many options out there, it’s essential to find a provider that meets your needs. Open Care Life Insurance has been gaining attention for its various offerings and competitive pricing. In this post, I’ll share what I’ve learned about Open Care, its legitimacy, coverage options, and what customers are saying about it.
What is Open Care Life Insurance?
Open Care Life Insurance is a provider that aims to offer affordable life insurance solutions tailored to individual needs. The company focuses on making life insurance accessible, with policies designed for families, young professionals, and anyone looking to secure their financial future. Whether you’re seeking term life insurance for temporary needs or whole life insurance for long-term coverage, Open Care has something for everyone.
Is Open Care Life Insurance Legit?
Licensing and Regulatory Compliance
One of the first things I look for when considering an insurance provider is legitimacy. Open Care Life Insurance holds the necessary licenses to operate in multiple states, which is a good sign. It’s always wise to verify this information through your state’s insurance department or the National Association of Insurance Commissioners (NAIC) to ensure the company is compliant with regulations.
Company Reputation
When I was researching Open Care, I found various customer reviews on platforms like the Better Business Bureau (BBB) and Trustpilot. Many customers praised the affordability and straightforwardness of their policies, while some voiced concerns about customer service experiences. However, it’s essential to consider that every company has its pros and cons. For instance, my neighbor recently shared her experience with Open Care, where she found the application process easy but had to follow up multiple times to get clarity on her policy.
Coverage Options Offered by Open Care
Open Care offers several types of life insurance policies, catering to different needs:
- Term Life Insurance: This type of policy provides coverage for a specified term, such as 10, 20, or 30 years. It’s often more affordable and is an excellent option for young families looking to cover expenses like a mortgage or children’s education.
- For Example: A close friend of mine opted for a 20-year term policy when he became a parent. He wanted to ensure his family would be financially secure in case anything happened to him during those crucial years.
- Whole Life Insurance: This provides lifelong coverage and builds cash value over time. It can be a good option for those looking for a more permanent solution.
- Universal Life Insurance: A flexible option that allows policyholders to adjust their premiums and death benefits. It’s ideal for those who want control over their insurance costs.
Additionally, Open Care offers riders, which are additional features that can enhance your coverage. For example, adding a critical illness rider can provide a payout if you’re diagnosed with a severe condition, which can be a lifesaver financially.
You may like: Plastic surgery insurance
Customer Experience with Open Care Life Insurance
Customer Service Quality
One of the most critical aspects of any insurance provider is customer service. From my research and conversations with others, Open Care has a mixed reputation in this area. Some customers reported satisfactory experiences, citing helpful representatives and quick responses, while others mentioned longer wait times and occasional difficulties in reaching support.
When I was considering my options for life insurance, I made a few calls to Open Care to ask questions about their policies. I found the representatives knowledgeable and willing to help, but I had to wait longer than I expected to get connected initially.
Claims Process
Filing a claim is often the most critical experience for policyholders. Based on various reviews, the claims process with Open Care can be straightforward if all documentation is in order. However, like with many providers, delays can occur, especially if paperwork is missing. A friend of mine had a smooth experience filing a claim after her mother passed away, but she also emphasized the importance of having all necessary documents prepared beforehand.
Cost and Affordability
Open Care Life Insurance is well-known for its competitive pricing, making it a suitable choice for those looking to save money on premiums. For example, I found their term life policies to be among the most affordable when comparing quotes from various providers.
Pricing Structure
While prices can vary based on age, health, and the type of coverage selected, Open Care generally provides reasonable rates. In my case, I received quotes for a term life policy that were lower than what I’d seen from some larger providers, which was a pleasant surprise.
Comparison to Competitors
When I compared Open Care with other insurers, it was evident that they stand out in terms of affordability. However, it’s essential to weigh the cost against factors like customer service and claims handling.
Pros and Cons of Open Care Life Insurance
Pros:
- Affordable Pricing: Great options for budget-conscious consumers.
- Diverse Coverage Options: Choices that cater to different needs and preferences.
- Easy Application Process: Many customers have reported a straightforward application experience.
Cons:
- Inconsistent Customer Service: While many have positive experiences, there are reports of long wait times.
- Limited Availability of Some Features: Depending on your state, some riders or features may not be available.
Who Should Consider Open Care Life Insurance?
Open Care Life Insurance may be ideal for:
- Young Families: If you’re looking for affordable term life insurance to protect your loved ones.
- Budget-Conscious Individuals: People who want reliable coverage without breaking the bank.
- Anyone Seeking Flexibility: Those interested in adjustable policies like universal life insurance.
In Short
Open Care Life Insurance presents a solid option for anyone looking to secure their financial future with affordable and straightforward life insurance products. While there are pros and cons to consider, it’s essential to weigh your unique needs against what Open Care offers. From my experience and research, it seems like a good fit for young families and those seeking budget-friendly options. As always, it’s wise to shop around and compare quotes to find the best coverage for you.
In the end, investing in life insurance is a crucial step toward financial security for you and your loved ones. Whether you choose Open Care or another provider, taking that step can provide peace of mind that’s invaluable.
FAQs about Open Care Life Insurance
- Is Open Care Life Insurance Legit?
Yes, Open Care is licensed to operate in several states and adheres to regulatory standards. - What Types of Coverage Does Open Care Offer?
They provide term life, whole life, and universal life insurance. - How Do I File a Claim with Open Care?
Claims can typically be filed through their customer service line or online portal. - Are There Additional Costs or Fees?
Standard premiums apply, but check for any specific fees related to policy management.

MyFastBroker Insurance Brokers guide to easy insurance
MyFastBroker Insurance Brokers is a company that helps people find the best insurance for their needs. Unlike many other brokers, MyFastBroker works with multiple insurance companies, offering clients a variety of options to choose from. The goal is to simplify the insurance process, making it less stressful and more affordable. Whether it’s for home, auto, health, or business insurance, MyFastBroker provides personalized assistance to ensure clients get the right coverage.

Why Choose an Insurance Broker?
Navigating the world of insurance can be confusing, especially with so many different plans and companies to consider. MyFastBroker Insurance Brokers takes the guesswork out of the process by comparing multiple providers and offering expert advice. This not only saves time but also helps clients secure better deals than they might find on their own. Instead of contacting different companies individually, MyFastBroker does all the legwork, providing a one-stop solution.
Services Offered by MyFastBroker
Personal Insurance
MyFastBroker assists with finding the best health, auto, home, and life insurance policies. For example, one recent case involved helping a family reduce their auto insurance costs while also improving their health coverage. MyFastBroker was able to save them money without sacrificing the quality of their insurance.Business Insurance
For business owners, MyFastBroker offers a range of commercial insurance services, including property and liability insurance, workers’ compensation, and industry-specific coverages. A small business owner was recently able to secure affordable coverage for their shop, ensuring their livelihood was protected against unforeseen events.Additional Services
In addition to offering various types of insurance, MyFastBroker provides assistance with filing claims and regularly reviews policies to ensure clients are still getting the best possible rates.Fast and Simple Service
MyFastBroker is known for its quick and easy service. The process of finding insurance is streamlined, so clients don’t have to worry about spending hours comparing plans. MyFastBroker works with multiple insurance providers, allowing clients to explore a variety of options in one place. The brokers at MyFastBroker are experienced professionals who guide clients step by step.
In one instance, a client needed health insurance quickly because their previous plan was about to expire. MyFastBroker was able to find a new plan that suited their needs within days, saving both time and money.
How MyFastBroker Works
The process at MyFastBroker follows four simple steps:
Step 1: Initial Consultation
The first step is to understand the client’s insurance needs. This could involve a phone call or an online consultation, where a broker will ask questions to assess the situation. Recently, a client was unsure about life insurance options. After a quick conversation, the broker was able to explain the different choices available, making the process clearer.Step 2: Customized Options
After understanding the client’s needs, MyFastBroker searches for policies from multiple companies. The options are then presented in a way that’s easy to compare, helping clients choose the best one for their situation.Step 3: Policy Selection and Purchase
Once the client has chosen a policy, MyFastBroker handles the rest, ensuring the insurance is set up quickly and securely. For example, a client recently needed insurance for a new car and was able to get coverage in less than an hour through this streamlined process.Step 4: Ongoing Support
Even after a policy is in place, MyFastBroker continues to support clients by offering reminders for renewals and assistance with any claims. When a family recently needed to file a claim for storm damage to their home, MyFastBroker ensured that the process went smoothly.Also Read: Harley Davidson insurance
Success Stories and Testimonials
MyFastBroker has a long history of helping clients find the right insurance. One example involves a single parent who was struggling to afford both health and car insurance. MyFastBroker was able to help them lower their premiums, allowing them to keep both policies without financial strain.
In another case, a bakery owner was concerned about what might happen if their business was affected by a fire or theft. MyFastBroker helped the owner find an affordable business insurance plan that offered full protection.
What Makes MyFastBroker Stand Out?
Personalized Service
MyFastBroker is dedicated to understanding each client’s unique needs, offering tailored insurance options rather than a one-size-fits-all approach.Expert Knowledge
With years of experience in the insurance industry, MyFastBroker has the knowledge and expertise to find the best policies for both individuals and businesses.Wide Range of Options
By working with many insurance companies, MyFastBroker is able to offer more choices than brokers who are limited to a single provider.Ready to Get Started?
For anyone looking for fast and easy insurance solutions, MyFastBroker is ready to help. Whether it’s for personal or business coverage, MyFastBroker offers tailored insurance options from multiple providers. Contact them today for a free quote and get started on finding the best insurance for your needs.
In Short
MyFastBroker Insurance Brokers takes the stress out of finding the right insurance. By offering expert guidance and multiple options from different companies, they ensure that clients receive the best coverage at the best price. Whether for home, health, auto, or business, MyFastBroker is committed to providing fast, personalized service every step of the way.
FAQs
- Is using a broker more expensive?
No. In fact, MyFastBroker often helps clients save money by finding the best deals from multiple providers. - How long does it take to get insurance through MyFastBroker?
In most cases, MyFastBroker can find and set up insurance in just a few days. - Can policies be changed later?
Yes, MyFastBroker can assist clients in switching to different policies if their needs change or if a better deal becomes available.
- Is using a broker more expensive?

Health insurance for plastic surgery coverage and costs explained
Plastic surgery is often perceived as a luxury, with many assuming that it falls entirely outside the scope of health insurance. While this is true for most cosmetic procedures, there are cases where health insurance can cover plastic surgery—particularly when it is deemed medically necessary.

This guide will walk you through the basics of how health insurance interacts with plastic surgery, the types of procedures that may qualify for coverage, and how you can navigate the complex world of insurance claims for surgical procedures.
Topic Key Points Types of Plastic Surgery – Cosmetic Surgery: Not typically covered by insurance.
– Reconstructive Surgery: Often covered if deemed medically necessary.Medically Necessary Procedures – Insurance covers surgeries like breast reconstruction, cleft lip repair, and rhinoplasty for breathing issues. Out-of-Pocket Costs – Cosmetic surgery costs: $3,500 – $12,000 depending on the procedure. Financing Options – Payment plans, medical credit cards, and third-party lenders. Steps for Insurance Coverage – Confirm with insurance provider.
– Get pre-authorization.
– Appeal denied claims if necessary.Supplemental Options – Supplemental insurance plans.
– Medical tourism (cost savings, but risks involved).article’s overview What Is Plastic Surgery?
Plastic surgery is a medical specialty that focuses on the repair, reconstruction, or alteration of the human body. It is divided into two primary categories:
- Cosmetic Surgery: These are elective procedures designed to enhance appearance. Examples include facelifts, liposuction, and breast augmentations. Health insurance typically does not cover cosmetic surgeries.
- Reconstructive Surgery: These procedures aim to correct deformities caused by accidents, medical conditions, or congenital disabilities. Surgeries like breast reconstruction after a mastectomy, cleft lip repair, and skin grafting after burns are some examples. Reconstructive surgeries are often covered by health insurance because they improve a person’s function or quality of life.
Types of Plastic Surgery Covered by Health Insurance
When discussing health insurance coverage for plastic surgery, the distinction between cosmetic and reconstructive surgery is crucial. Insurance companies tend to cover procedures that are considered medically necessary. But how is medical necessity defined?
Medical Necessity: The Key to Insurance Coverage
Health insurance providers typically cover reconstructive surgeries if they are needed to restore normal function, relieve pain, or correct defects that affect a person’s quality of life. The term medical necessity is the deciding factor for whether a procedure will be covered.
Some examples of plastic surgeries that are often covered by insurance when deemed medically necessary include:
- Breast reconstruction after mastectomy.
- Rhinoplasty to correct breathing problems due to a deviated septum.
- Eyelid surgery (blepharoplasty) if drooping eyelids impair vision.
- Skin grafting following severe burns.
However, for insurance to approve coverage, the patient must provide medical documentation that demonstrates the need for the surgery. This may include tests, doctor’s notes, and other forms of evidence showing that the procedure is not purely cosmetic.
Common Reconstructive Procedures Covered by Insurance
Let’s take a closer look at some of the reconstructive surgeries typically covered by insurance:
- Breast Reconstruction: Women who have undergone mastectomies as part of breast cancer treatment are entitled to breast reconstruction coverage under the Women’s Health and Cancer Rights Act (WHCRA). This law mandates that health insurance companies cover breast reconstruction surgeries, including nipple reconstruction and symmetry procedures for the other breast.
- Cleft Lip and Palate Surgery: Children born with cleft lips or palates often require multiple surgeries to correct their appearance and improve their ability to speak and eat. These surgeries are generally covered by insurance due to the impact on the child’s health and development.
- Deviated Septum Correction: While rhinoplasty for cosmetic reasons is rarely covered by insurance, a deviated septum that impairs breathing may qualify as medically necessary. In these cases, insurance will typically cover the part of the surgery related to correcting the septum, but not necessarily any cosmetic modifications.
When Plastic Surgery Costs Fall on You
In many cases, patients must bear the costs of plastic surgery themselves, especially for elective cosmetic procedures that are not considered medically necessary. Understanding the potential costs involved can help you make informed decisions if your surgery isn’t covered by insurance.
Out-of-Pocket Costs for Common Cosmetic Procedures
Cosmetic surgeries are typically paid out-of-pocket by the patient, as insurance companies view these procedures as elective, and they do not address medical or functional concerns. The costs for cosmetic surgeries can vary widely based on the complexity of the procedure, the surgeon’s expertise, and the location of the practice. Here are some average costs of popular cosmetic surgeries:
- Breast Augmentation: $6,000 – $8,000
- Liposuction: $3,500 – $7,000
- Facelift: $7,000 – $12,000
- Tummy Tuck (Abdominoplasty): $6,000 – $10,000
These prices often do not include additional costs like anesthesia, operating room fees, and post-surgery medications, which can add up quickly.
Financing Options for Cosmetic Surgery
If you’re considering a cosmetic surgery that isn’t covered by insurance, there are several financing options to help make the costs more manageable:
- Payment Plans: Many plastic surgeons offer in-house financing options or partner with third-party lenders to provide installment payment plans. These allow you to spread the cost of your surgery over several months or years.
- Medical Credit Cards: Some companies offer credit cards specifically designed for medical expenses. These cards often come with promotional 0% interest rates for a set period, making it easier to pay for your surgery without incurring high-interest charges.
Navigating Health Insurance for Plastic Surgery
If your surgery may qualify for insurance coverage, understanding the process can be challenging. Here are some steps to help you navigate insurance claims for plastic surgery:
Confirm Coverage with Your Insurance Provider
Before scheduling any surgery, it’s essential to contact your health insurance provider to verify coverage. When speaking with an insurance representative, ask the following questions:
- Is this procedure covered under my plan?
- What documentation do I need to submit for approval?
- Does the procedure require pre-authorization?
It’s also helpful to get any approvals or denials from the insurance company in writing, so you have a clear record of their decision.
Appealing a Denied Claim
If your insurance company denies coverage for a procedure that you believe is medically necessary, you have the right to appeal their decision. The appeals process can be time-consuming, but it’s worth pursuing if you believe the surgery is essential for your health and well-being. To strengthen your appeal, consider getting a second opinion from another physician who can support your claim.
Supplemental Insurance and Medical Tourism
If traditional health insurance doesn’t cover the plastic surgery you need, there are alternative ways to manage the costs.
Supplemental Insurance for Elective Procedures
Some companies offer specialized supplemental insurance plans that cover elective plastic surgery. These policies can help pay for cosmetic procedures not covered by traditional insurance, although premiums may be high.
Medical Tourism: Is It Worth the Risk?
Some patients choose to travel abroad for plastic surgery, as costs can be significantly lower in countries like Mexico, Thailand, or Brazil. While medical tourism can save money, it carries risks, including potential complications, lack of legal recourse, and differing medical standards. Before opting for surgery abroad, thoroughly research the credentials of the surgeon and facility, and ensure they meet international safety standards.
Conclusion
Navigating the world of health insurance and plastic surgery can be confusing, but understanding the difference between cosmetic and reconstructive procedures is key to determining coverage. While most cosmetic surgeries are not covered by insurance, medically necessary reconstructive procedures often are. Always consult both your plastic surgeon and your insurance provider before undergoing any surgery, and explore your options for financing if insurance won’t cover the cost. Planning ahead and being informed will help ensure that your experience is as smooth and stress-free as possible.
FAQs
1. Does health insurance cover cosmetic surgery?
No, health insurance typically does not cover cosmetic surgery since these procedures are considered elective and not medically necessary.2. What types of plastic surgery are covered by insurance?
Reconstructive surgeries, such as breast reconstruction after a mastectomy, cleft lip repair, and surgeries to correct breathing issues, may be covered if deemed medically necessary.3. How can I determine if my plastic surgery will be covered?
Contact your health insurance provider to verify coverage. Ask about pre-authorization and what documentation is required to prove medical necessity.4. What should I do if my insurance claim for plastic surgery is denied?
You have the right to appeal a denied claim. Gather supporting documentation, potentially including a second opinion from another doctor, and follow your insurer’s appeal process.5. Are there financing options available for cosmetic surgery?
Yes, many plastic surgeons offer payment plans, and there are medical credit cards and third-party lenders that can help finance cosmetic procedures.6. What is medical necessity in relation to plastic surgery?
Medical necessity refers to procedures that are essential for improving a patient’s health or quality of life, which can qualify for insurance coverage.
Massage therapy coverage health insurance insights
Massage therapy is widely recognized for its health benefits, ranging from relaxation to pain relief and rehabilitation. As more people turn to massage for their wellness needs, an important question arises: Can health insurance cover massage therapy? While the answer is not always straightforward, understanding the nuances of health insurance coverage for massage can save time, money, and confusion.

This blog aims to break down how health insurance can work with massages therapy, the steps to secure coverage, and what to do if your plan doesn’t cover it.
Topic Key Information Health Benefits of Massage Pain relief, stress reduction, improved circulation, rehabilitation, and faster recovery from injuries. Insurance Coverage Depends on medical necessity, type of insurance, and specific policy terms. Conditions for Coverage Chronic pain, injury recovery, musculoskeletal disorders, surgery rehabilitation (with doctor’s referral). Types of Insurance Private health insurance, Medicare/Medicaid (limited), Workers’ Compensation, FSAs/HSAs. Steps to Secure Coverage Check policy, get doctor’s referral, verify coverage with insurer, submit claims. Potential Barriers Limited sessions, out-of-network therapists, denied claims due to insufficient documentation. Costs Without Insurance Average cost: $60-$120 per session. Membership plans and discounts may reduce costs. Alternatives Membership plans, community clinics, discounted student massages, online deals (e.g., Groupon). overview of the article The Role of Massage Therapy in Health and Wellness
Massage therapy is more than a luxury spa treatment. It has been used for centuries as a therapeutic practice to address a variety of physical and emotional issues. Modern Massage treatment involves techniques that manipulate muscles, soft tissues, and joints to relieve pain, reduce stress, and enhance overall well-being.
Common types of massage include:
- Swedish massage: Focuses on relaxation and gentle techniques.
- Deep tissue massage: Targets muscle knots and chronic tension.
- Sports massage: Helps athletes recover from injuries and improve performance.
- Trigger point therapy: Relieves specific areas of muscle tightness that cause pain in other parts of the body.
The benefits of massage therapy go beyond relaxation. It has been shown to:
- Alleviate chronic pain.
- Reduce inflammation.
- Improve circulation.
- Promote faster recovery from injuries.
- Decrease stress and anxiety.
Given these benefits, many people seek Massage treatment as part of their regular healthcare routine. But does your health insurance recognize it as a valid medical treatment?
Health Insurance and Massage Therapy: What to Know
Health insurance policies typically cover treatments deemed medically necessary, but massage treatment often occupies a gray area between medical care and alternative therapy. Whether or not your insurance plan covers massage treatment depends on several factors, including the nature of your health condition, your insurance provider, and the specifics of your policy.
In general, massage therapy is more likely to be covered by insurance if it is prescribed by a healthcare provider, such as a doctor or physical therapist, for a specific medical condition. For example, individuals recovering from surgery, managing chronic pain, or undergoing rehabilitation for an injury may have a better chance of securing coverage for massage therapy.
When Can Massage Therapy Be Covered?
To increase your chances of having massage therapy covered by your insurance, it’s essential to meet certain criteria. The first requirement is typically a diagnosis or medical condition that justifies the treatment. Common conditions for which massage may be covered include:
- Chronic pain: Individuals with long-term pain due to conditions like fibromyalgia, arthritis, or back issues may qualify.
- Injury recovery: Massage therapy can be part of a treatment plan following surgery or trauma.
- Rehabilitation: After a stroke or injury, massage therapy can aid in regaining mobility and function.
- Musculoskeletal disorders: Issues like carpal tunnel syndrome or tendonitis may also justify coverage.
In most cases, you’ll need a doctor’s referral or prescription for massage therapy. Without this, insurers are less likely to approve the treatment as medically necessary. This referral must outline the diagnosis, recommended number of sessions, and expected outcomes from the therapy.
Also Read: Health Insurance for Weight Loss Surgery
Health Insurance Plans and Massage Coverage
Understanding the type of health insurance you have is critical in determining whether massage therapy will be covered. Here’s a quick overview of how different insurance plans may approach massage coverage:
- Private health insurance: Some private insurers may offer limited coverage for massage therapy under specific conditions, but it largely depends on the plan’s terms. HMO (Health Maintenance Organization) plans typically have more restrictions than PPO (Preferred Provider Organization) plans.
- Medicare and Medicaid: Unfortunately, massage therapy is rarely covered under Medicare or Medicaid unless it is deemed absolutely medically necessary, and even then, coverage is highly restrictive. You’ll need to consult with your provider to determine eligibility.
- Worker’s compensation: If you’ve been injured on the job and massage therapy is part of your recovery plan, your worker’s compensation insurance may cover it. However, you’ll need medical documentation that links the therapy directly to your work injury.
- FSA and HSA accounts: Even if your primary insurance doesn’t cover massage therapy, you might still be able to use Flexible Spending Accounts (FSA) or Health Savings Accounts (HSA) to pay for it. These accounts allow you to set aside pre-tax dollars for medical expenses, which may include massage therapy when prescribed by a doctor.

How to Get Massage Therapy Covered by Health Insurance
Navigating health insurance can be tricky, especially when it comes to alternative treatments like massage therapy. However, with some diligence, you can improve your chances of securing coverage. Here’s a step-by-step guide to follow:
- Check your insurance policy: Before anything else, review your insurance plan’s details. Look for specific mentions of alternative therapies, rehabilitation services, or physical therapy benefits. If it’s not clear, contact your insurance provider to ask if massage therapy is covered for your specific condition.
- Get a referral or prescription: If you believe you need massage therapy for a medical reason, consult your healthcare provider. You’ll need them to diagnose the condition and provide a prescription or referral that outlines why massage is necessary, how it will help, and the number of sessions recommended.
- Contact your insurer: After securing the doctor’s recommendation, call your insurance company to verify that they will cover the therapy. Ask about the required documentation, whether you need to use an in-network provider, and any limitations on coverage, such as the number of sessions allowed.
- Submit claims: If your insurer covers massage therapy, keep detailed records of your sessions, referrals, and any paperwork from your healthcare provider. Submit your claims promptly and follow up to ensure they are processed correctly.
Barriers to Massage Coverage
Even with a referral, getting health insurance to cover massage therapy is not always straightforward. Here are some common obstacles you may encounter:
- Coverage limitations: Some plans may only cover a set number of sessions, or they might limit the type of massage that is covered (e.g., only rehabilitative massage, not relaxation).
- Out-of-network providers: If the therapist you want to see is not part of your insurer’s network, you may face higher out-of-pocket costs or outright denial of coverage.
- Denied claims: Insurers may deny your claim if they believe the massage therapy is not medically necessary or if there is incomplete documentation. Always ensure that your doctor provides thorough information on why the treatment is needed.
Costs Without Insurance Coverage
If your health insurance doesn’t cover massage therapy, you’ll need to pay out of pocket. The cost of massage therapy varies widely depending on the type of massage, location, and the therapist’s experience. On average, a one-hour massage session can cost between $60 and $120.
While this can add up, it’s essential to weigh the benefits of the therapy against the costs. Some massage clinics offer membership plans or discounts for regular clients, which can help reduce the financial burden.
Alternatives to Insurance-Covered Massage
If your insurance won’t cover massage therapy, there are other ways to make it more affordable. Consider these options:
- Membership plans: Many spas and massage clinics offer discounted rates for members who sign up for monthly sessions.
- Community clinics: Some massage therapy schools or community health centers offer discounted massages performed by students or at a reduced rate to make therapy more accessible.
- Online deals: Websites like Groupon often offer discounted massage services.
Final Thoughts
Massage therapy is a valuable part of healthcare for many individuals, but insurance coverage is often limited. The key to getting your therapy covered is understanding your health insurance plan, obtaining a doctor’s referral, and following up with your insurer to clarify the terms. Whether or not your insurance covers it, massage therapy can be a worthwhile investment in your health and well-being.

Is Laser Eye Surgery Covered by Health Insurance? Find Out!
Laser eye surgery, such as LASIK or PRK, has revolutionized vision correction, offering people the chance to say goodbye to glasses and contact lenses. However, while the promise of clear vision is appealing, one critical question remains for many prospective patients: Does health insurance cover laser eye surgery?

This question often plays a decisive role in whether people proceed with the procedure, as the cost of eye surgery can be significant. In this blog post, we will dive deep into what eye surgery entails, why insurance coverage can be complicated, and what alternatives exist for financing the procedure.
Topic Key Details Laser Eye Surgery Overview Common procedures: LASIK, PRK, SMILE; used to correct myopia, hyperopia, astigmatism. Insurance Coverage Usually classified as elective, hence not covered by most health insurance. Private Health Insurance May offer limited coverage or discounts through vision riders. Employer Health Plans (FSA/HSA) Use pre-tax dollars to cover laser surgery costs via Flexible or Health Savings Accounts. Government Programs Medicare and Medicaid generally do not cover elective laser eye surgery. Financing Alternatives Payment plans, clinic promotions, military/union discounts can help manage costs. Key Tips for Insurance Contact insurance, get pre-authorization, and request itemized quotes for costs. overview of the article What is Laser Eye Surgery?
Laser eye surgery, particularly LASIK (Laser-Assisted in Situ Keratomileusis), is a widely recognized procedure designed to correct vision problems like nearsightedness (myopia), farsightedness (hyperopia), and astigmatism. The surgery uses precise lasers to reshape the cornea, allowing light entering the eye to be correctly focused onto the retina, resulting in improved vision.
While LASIK is the most common form of eye surgery, others, such as PRK (Photorefractive Keratectomy) or SMILE (Small Incision Lenticule Extraction), serve similar purposes. These surgeries are often quick, with relatively short recovery times and high success rates. For many people, they offer the prospect of a life free from glasses or contacts.
But with a procedure that can cost between $2,000 to $4,000 per eye, many wonder whether their health insurance will cover this potentially life-changing surgery.
The Health Insurance Dilemma: Is Laser Eye Surgery Covered?
The short answer is: Not usually. Most health insurance companies classify eye surgery as an elective procedure, which means it is not deemed medically necessary. In contrast to surgeries needed to restore bodily functions or treat illness, elective procedures are those that are chosen for personal reasons, even if they improve quality of life.
For the majority of patients, laser eye surgery falls into this category. Glasses and contact lenses are viewed as adequate solutions to vision problems by most insurance providers, making eye surgery an optional procedure rather than a medical necessity.
However, there are exceptions. In rare cases where refractive errors are so severe that they impair normal vision even with corrective lenses, some insurance plans may provide partial or full coverage. For example, if a patient has extreme vision problems that significantly affect their ability to work or function in daily life, a doctor may be able to prove that the surgery is necessary, making the case for insurance coverage.
Nevertheless, these instances are rare, and the burden of proving the surgery is medically necessary is often on the patient.
Private Health Insurance and Laser Eye Surgery
Private health insurance policies can vary widely, but generally, they follow the same guidelines: unless a doctor provides evidence that the surgery is medically required, it won’t be covered.
However, some insurance companies do offer vision plans or riders that can be added on to existing health insurance coverage. These plans are specifically designed to cover vision-related procedures, but they still may not include eye surgery as a covered benefit. It’s important to read the fine print, as many vision plans cover routine eye exams, prescription lenses, and corrective eyewear, but not elective surgeries.
In cases where vision riders do cover part of the cost of laser eye surgery, the coverage is typically limited. For instance, some plans may offer a discount on the total cost of surgery rather than paying for it outright.
Employer Health Plans: FSA and HSA
For many people, employer-sponsored health plans may not directly cover eye surgery, but they offer indirect ways to manage the cost. Two popular options are Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA).
These accounts allow employees to set aside pre-tax dollars to cover medical expenses, which can include eye surgery. By using funds from an FSA or HSA, patients can reduce their taxable income, making eye surgery more affordable. This is a particularly attractive option for those who are set on getting the procedure but don’t have direct insurance coverage for it.
Also Read: Does Insurance Cover Wisdom Teeth Removal
Government Health Insurance: Medicare and Medicaid
If you’re relying on government health insurance programs like Medicare or Medicaid, it’s unlikely that they will cover laser eye surgery. Medicare, for instance, covers medical services that are necessary to treat health conditions, but it does not usually cover elective procedures. However, Medicare will cover certain eye surgeries that are medically necessary, such as cataract surgery, but eye surgery for refractive errors is typically excluded.
Medicaid rules vary by state, but generally, it also does not cover elective surgeries like LASIK.
Financing Alternatives: Payment Plans and Discounts
For those who don’t have insurance coverage for laser eye surgery, several alternative financing options can make the cost more manageable.
Many eye clinics and surgery centers offer financing plans. These plans allow patients to spread the cost of surgery over time, often with low or no interest for a certain period. Financing can help make the immediate cost of surgery less daunting, especially when paid in monthly installments. Be sure to ask your clinic about their financing options, as terms can vary widely.
Some providers also offer discount programs or promotional rates. Military members, union workers, and even employees of certain companies may qualify for discounted rates on eye surgery. Clinics may run seasonal promotions or provide discounted rates for referrals or repeat patients.
Finally, using your FSA or HSA funds can help offset the cost of laser surgery. These accounts are designed to be used for medical expenses, and while the surgery may not be covered by insurance, it qualifies as an eligible expense for FSA and HSA funds.
Checking Your Health Insurance for Laser Eye Surgery Coverage
Before scheduling any eye surgery, it’s essential to check with your insurance provider and get a clear understanding of what, if any, coverage you have. Here’s a step-by-step guide:
- Contact your insurance company: Ask about specific policies regarding laser eye surgery. Make sure to inquire whether the procedure is considered elective or medically necessary in your situation.
- Get pre-authorization: If your doctor believes that your surgery may be medically necessary, make sure you get pre-authorization from your insurance provider. This step is crucial to avoid unexpected costs after surgery.
- Ask for an itemized quote: Laser eye surgery clinics should provide a detailed quote of the expected costs. This will help you compare the out-of-pocket cost with what your insurance might cover.
Final Considerations for Laser Eye Surgery
While the prospect of improved vision is enticing, deciding whether to undergo laser eye surgery requires careful consideration. Beyond the cost, it’s important to think about the long-term benefits and risks of the surgery.
While laser eye surgery is generally considered safe, it does carry risks like any surgical procedure. Potential complications include dry eyes, glare, or vision issues that could require follow-up surgeries. It’s also essential to understand that not everyone is an ideal candidate for laser eye surgery, and a thorough consultation with an experienced ophthalmologist is necessary before making your decision.
Conclusion
For most patients, laser eye surgery is considered an elective procedure, and as such, health insurance doesn’t usually cover it. However, by exploring your options—such as employer-sponsored FSAs or HSAs, payment plans, or potential discounts—you can find ways to make the surgery more affordable.
Before making any decisions, check with your insurance provider, understand the total cost, and weigh the long-term benefits against the immediate financial burden. Laser eye surgery can be life-changing, but it’s important to go into it with your eyes wide open—both literally and financially.

Health Insurance for Weight Loss Surgery
Weight loss surgery, also known as bariatric surgery, can be a life-changing solution for individuals struggling with severe obesity and its related health complications. However, one of the major hurdles many people face is the financial burden of the procedure. Health insurance can play a crucial role in making this type of surgery more accessible.
In this blog, we’ll dive deep into what you need to know about health insurance for weight loss surgery, the approval process, and how to navigate potential denials.
Topic Key Information Weight Loss Surgery Medical procedure to treat severe obesity (e.g., gastric bypass, sleeve gastrectomy). Health Insurance Coverage Most major insurers, Medicaid, and Medicare may cover surgery under specific conditions. Requirements for Coverage BMI over 40, or 35 with obesity-related conditions; documentation of failed weight loss attempts. Pre-Approval Process Medical evaluation, supervised weight loss program, nutritional and psychological evaluations. Maximizing Insurance Approval Stay organized, work with bariatric specialists, understand co-pays and deductibles. Dealing with Denials File an appeal with additional medical documentation and support from your doctor. Alternatives to Insurance Self-pay, medical tourism, financial assistance programs. Future of Coverage Growing advocacy for wider insurance coverage and recognition of bariatric surgery as a necessary intervention. an overview of the article Understanding Weight Loss Surgery and Its Importance
Weight loss surgery is not just about shedding pounds for cosmetic reasons. It’s a medical intervention designed to help individuals with obesity, particularly those whose health is at risk due to excess weight. Obesity is often linked to serious conditions such as type 2 diabetes, heart disease, high blood pressure, and sleep apnea. For many, bariatric surgery is a last resort after years of unsuccessful dieting, exercise programs, and lifestyle changes.
Several types of weight loss surgeries exist, with gastric bypass and sleeve gastrectomy being among the most common. These surgeries alter the digestive system to reduce food intake or nutrient absorption, leading to significant weight loss. However, because these procedures are complex and require long-term follow-up care, they can be costly without insurance coverage.
Does Health Insurance Cover Weight Loss Surgery?
One of the first questions many people ask is, “Does my health insurance cover weight loss surgery?” The answer depends on several factors, including your specific insurance plan and whether you meet the medical criteria for surgery.
Most major insurance providers, including employer-sponsored health plans, Medicaid, and Medicare, do offer coverage for bariatric surgery under certain conditions. However, not all plans automatically include weight loss surgery as part of their coverage. It’s essential to review your plan details or speak with your insurance provider to confirm whether you’re eligible.
Requirements for Health Insurance Coverage of Weight Loss Surgery
While many insurance plans do cover weight loss surgery, there are typically strict requirements to qualify for coverage. Insurance companies often label bariatric surgery as a “medically necessary” procedure, meaning it must be deemed essential for your health rather than elective.
To qualify for coverage, you’ll usually need to meet certain medical criteria. These criteria often include having a body mass index (BMI) over 40, or over 35 if you also suffer from obesity-related conditions like diabetes, heart disease, or high blood pressure. Some plans may also require proof of unsuccessful attempts at non-surgical weight loss methods, such as diet and exercise programs.
Additionally, your insurance provider may ask for documentation, such as a history of weight-related medical issues, a referral from your doctor, or records of medically supervised weight loss attempts.
The Pre-Approval Process for Bariatric Surgery
Before you can undergo weight loss surgery, you’ll need to go through a pre-approval process with your insurance company. This process ensures that you meet the necessary qualifications and that your insurance will cover the surgery costs.
Here’s a breakdown of the common steps involved:
- Medical Evaluation: Your doctor will evaluate your health to determine if bariatric surgery is a suitable option. This evaluation includes reviewing your BMI, medical history, and any related health conditions.
- Supervised Weight Loss Program: Many insurance companies require you to participate in a medically supervised weight loss program before approving surgery. These programs often last several months and are designed to show that you’ve made efforts to lose weight without surgery.
- Nutritional and Psychological Evaluations: Insurers typically require you to meet with a nutritionist and undergo a psychological evaluation to ensure you understand the lifestyle changes required post-surgery and are mentally prepared for the procedure’s demands.
- Insurance Pre-Authorization: Once all required documentation and evaluations are complete, your doctor’s office will submit a pre-authorization request to your insurance company. This request includes detailed medical information and justifications for why the surgery is necessary.
The pre-approval process can take weeks or even months, so it’s essential to start early and work closely with your healthcare provider to gather all the necessary documentation.
Also Read: Does Insurance Cover Wisdom Teeth Removal
Maximizing Your Chances of Insurance Approval
Navigating the health insurance process for weight loss surgery can be complex, but there are steps you can take to improve your chances of getting approved:
- Stay Organized: Keep thorough records of all medical evaluations, diet attempts, and required appointments. Having organized documentation will make it easier to meet your insurance provider’s requirements.
- Work with a Bariatric Surgeon’s Office: Many bariatric surgery practices have insurance specialists who are familiar with the approval process. They can help you navigate the steps, ensuring you meet all the requirements and submit the necessary paperwork.
- Understand Your Insurance Plan: Review your plan to understand what is covered, including co-pays, deductibles, and any out-of-pocket costs you may incur. Knowing the financial side of things upfront will help you prepare for any expenses that arise.
- Consider Alternative Options: If your insurance doesn’t cover a particular procedure or has strict requirements, you may want to explore alternatives, such as changing your insurance plan during open enrollment or looking into a supplemental insurance policy.
Dealing with Insurance Denials and the Appeal Process
Unfortunately, not all insurance claims for weight loss surgery are approved on the first try. It’s common to face initial denial, but that doesn’t mean the door is closed. Denials can happen for several reasons, such as insufficient documentation or failure to meet certain medical criteria.
If your claim is denied, it’s crucial to act quickly and follow your insurance company’s appeal process. Most insurers have a structured process that allows you to contest their decision by providing additional information or clarifications. This may involve submitting more medical evidence, a letter of medical necessity from your doctor, or completing additional weight loss programs.
Working with a healthcare advocate or legal professional can also increase your chances of a successful appeal if you’re having trouble navigating the process.
What to Do If Your Insurance Doesn’t Cover Weight Loss Surgery
If your insurance plan does not cover weight loss surgery, there are still several options to consider:
- Self-Pay: Some individuals choose to pay for the surgery out of pocket. Many bariatric surgeons offer financing plans or payment options to make this more feasible. However, this can be costly, with prices ranging from $15,000 to $25,000 or more.
- Medical Tourism: Traveling abroad for weight loss surgery is another option. Countries like Mexico, Costa Rica, and India offer bariatric surgery at a fraction of the cost compared to the U.S. However, there are risks associated with medical tourism, including language barriers, follow-up care challenges, and potential complications.
- Financial Assistance Programs: Some hospitals and clinics offer financial assistance or charity care programs for patients who qualify. You may also find non-profit organizations that provide grants or financial aid for bariatric surgery.
The Future of Weight Loss Surgery and Health Insurance
As awareness of obesity as a public health issue grows, there are signs that insurance coverage for weight loss surgery may expand. Advocacy groups are working to ensure that more insurance companies recognize bariatric surgery as a necessary medical intervention rather than an elective procedure.
Changes in healthcare legislation and policy, such as the Affordable Care Act, have also increased access to bariatric surgery for many individuals. As the conversation around obesity evolves, it’s likely that more people will gain access to the treatments they need to live healthier lives.
Final Thoughts
Health insurance can be a game-changer when it comes to accessing weight loss surgery. However, understanding your insurance plan, meeting medical criteria, and navigating the approval process are essential steps to ensuring your surgery is covered. By being proactive, staying organized, and working closely with your healthcare provider, you can improve your chances of getting insurance approval and embarking on your weight loss journey with confidence.